-
What is Diabetes
Diabetes mellitus is a chronic disease characterised by high blood sugar due to problems with the hormone insulin. Insulin works like a key that unlocks all the cells of our body so that glucose from the food we eat can get inside and be converted into energy to power our muscles and organs. Diabetes affects 415 million people worldwide, causing an estimated 5 million deaths every year.
There are two main types of diabetes. Type I diabetes (T1D) is not currently preventable and is an autoimmune disease that affects approximately 10% of diabetes patients. In Type I diabetes the body’s own immune system destroys the cells in the pancreas that produce insulin. Type I diabetes patients need to take insulin injections every day to survive as their body no longer produces insulin. It is usually diagnosed in childhood.
Type II diabetes (T2D) affects approximately 90% of patients. It is often, but not always associated with being overweight or obese and it is preventable in most cases, by implementing a healthy diet and regular exercise. In Type II diabetes insulin is produced, but does not work as it should because the body is resistant to its action. Over time, the patients may need insulin injections and oral medications to manage their disease, as the insulin produced reduces or the body becomes more resistant to its action.
Constant high blood sugar has many negative effects including:
- Retinopathy (damage to blood vessels in the eye, which can lead to blindness )
- Nephropathy (damage to the kidneys, which can lead to renal failure )
- Neuropathy (damage to nerves, which can lead to loss of balance, numbness and diabetic foot disease ; swelling, ulceration and infection of the foot which may necessitate amputation)
- Cardiovascular disease (which kills 50% of people with diabetes)
Read more about diabetes…
-
What is insulin therapy
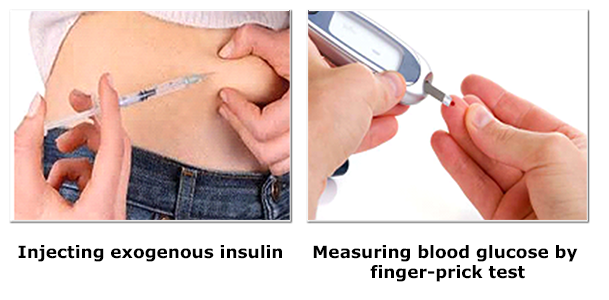
Exogenous insulin administration
Insulin therapy has proven effective for the management of T1D and insulin-dependent T2D, but requires onerous monitoring of blood glucose to prevent hypoglycaemia (low blood sugar). If too much insulin is injected it can result in a lack of sugar in the blood, which can be very dangerous as the brain needs a constant supply to function correctly and remain conscious. For this reason diabetes patients must use blood glucose meters to monitor their levels before injecting at least 4 times a day.
-
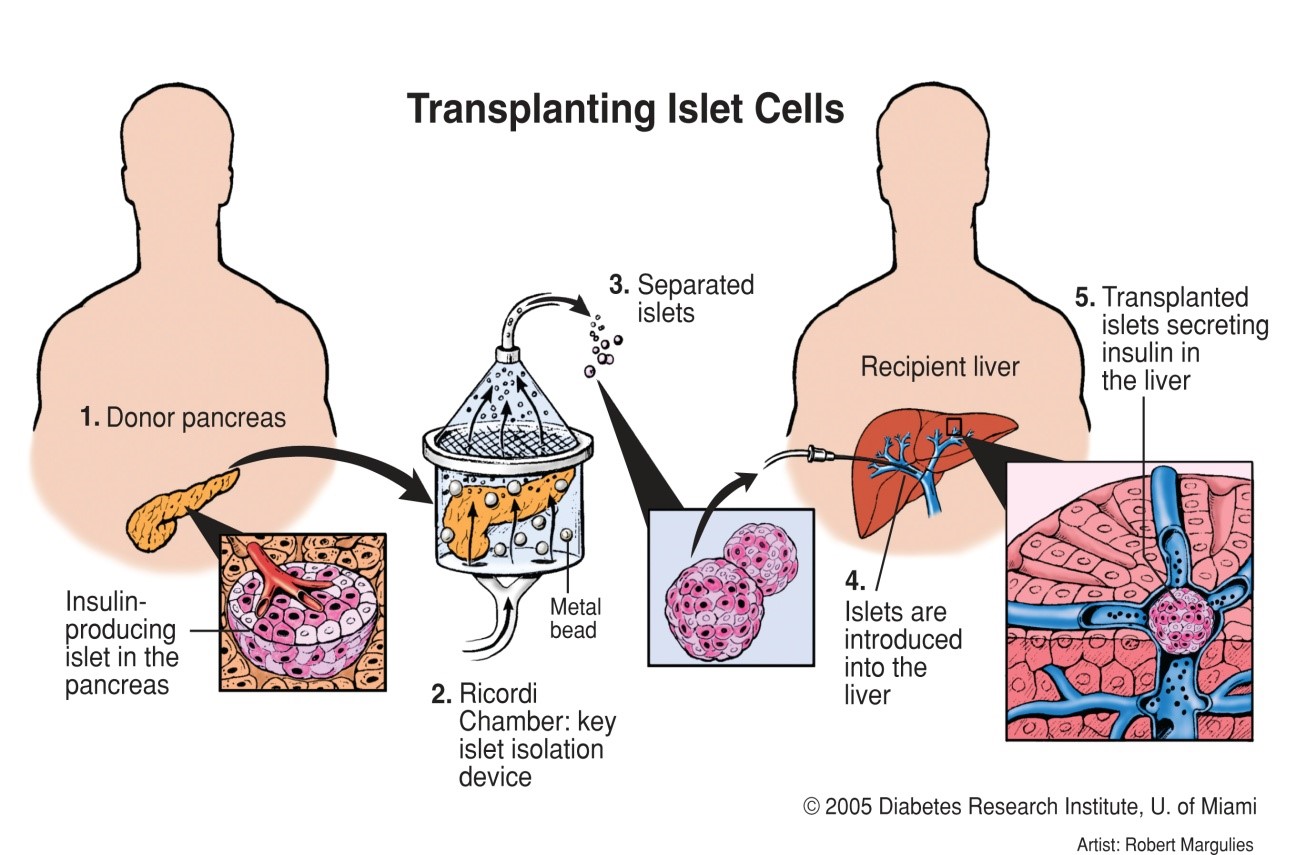
Islet transplantation
is a very promising therapy that has the potential advantage of re-establishing naturally-regulated insulin production. With this technique, pancreatic islets are harvested from donor pancreases and delivered to the liver by a catheter via the portal vein. Once in the liver the islets engraft and begin to produce insulin in response to blood glucose levels.
Following islet transplant, 50% of patients do not need to take insulin injections for 5 years or more and never again have dangerous unaware hypoglycaemic attacks. However, many islets are lost during and after transplantation due to lack of suitable support matrix, lack of an early oxygen supply and unfavourable inflammatory conditions within the blood vessels of the liver. As a consequence, 2-3 donor pancreases are needed to get enough islets to reverse diabetes. Furthermore, the patient must take lifelong immunosuppressive medications, which have significant negative side effects and therefore islet transplant therapy is currently only approved for the most at risk “brittle” T1D patients , or patients already on immunosuppression.
-
Challenges
The main challenge for DRIVE is to improve pancreatic islet transplant therapy for diabetes mellitus achieving sufficient delivery, retention and maintaining survival, engraftment and functioning of newly implanted islets. DRIVE will prevent the main factors contributing to islet graft loss.
The challenge The DRIVE solution Hypoxia due to inadequate early vascularisation β-Gel contains oxygen producing compounds thus supplying the islets with oxygen over the first week while they are most vulnerable Insufficient retention due to lack of a suitable support matrix β-Gel is a pancreo-mimetic gel that provides a suitable support matrix to the islets Inadequate extracellular matrix (ECM) cues at the site of transplantation Specific ECM molecules acting as efficacy cues will be included in the β-Gel Inflammatory reaction at the delivery site β-Shell will be a protective and retentive capsule for the delivery of islets outside the hostile liver environment Allo- and autorejection The implants will be immunoprotective and will carry efficacy cues with controllable release to potentiate the survival and decrease the time to efficacy of the islets
DRIVE